“`html
Effective Ways to Get Rid of Fungal Acne: Proven Tips for Healthy Skin in 2025
Fungal acne, a term commonly used to describe folliculitis caused by the yeast Malassezia, can be a frustrating condition for many. Unlike regular acne, it often presents as itchy, inflamed bumps that are easily confused with hormonal breakouts. In this article, we will explore effective fungal acne treatment options, natural remedies, and proper skincare routines to help you eliminate fungal acne and achieve clear, healthy skin.
Understanding Fungal Acne
Before we delve into solutions, it’s essential to understand the **causes of fungal acne**. Predominantly triggered by an overgrowth of yeast, particularly after sweating or wearing occlusive clothing, understanding how this condition differs from regular acne can significantly impact your treatment strategies. Fungal acne manifests as small, red papules, often appearing on the chest and back, and frequently worsens in hot, humid environments. Recognizing the **signs of fungal acne** early on can prevent prolonged inflammation and scarring.
Fungal Acne vs Regular Acne
Knowing the difference between fungal acne and regular acne is crucial for treatment. **Fungal acne**, or Malassezia folliculitis, occurs when the natural yeast on your skin proliferates uncontrollably. This condition is often characterized by itchy bumps that may cluster together. In contrast, **regular acne** is caused primarily by oil, bacteria, and clogged pores. Understanding these differences can help in selecting the right **fungal acne treatment**. Regular acne medications like benzoyl peroxide can exacerbate fungal acne, while antifungal creams can provide relief.
How to Identify Fungal Acne
Identifying fungal acne can save time and prevent unnecessary treatments. Here are a few steps to recognize it:
1. **Appearance**: Look for uniform, small, and red bumps that may run together.
2. **Itching and irritation**: If your acne is itchy, it may be fungal.
3. **Location**: Common areas include the chest, back, and shoulders, places prone to sweating.
If you’re unsure, consulting a dermatologist for a professional diagnosis is always advisable.
Common Misconceptions about Fungal Acne
There are several **common misconceptions** about fungal acne that can mislead treatment efforts. Many people believe yeast infections only occur in private areas, but skin can also suffer from overgrowth anywhere, producing **fungal acne symptoms**. Others may think that all acne treatments are suitable for fungal issues; however, many popular acne products contain pore-clogging ingredients that exacerbate fungal conditions. Debunking these myths is essential for effective management.
Effective Treatments for Fungal Acne
When it comes to treating fungal acne, various options exist, ranging from over-the-counter products to professional treatments. It’s crucial to consider individual skin types and the severity of the condition when selecting a treatment plan.
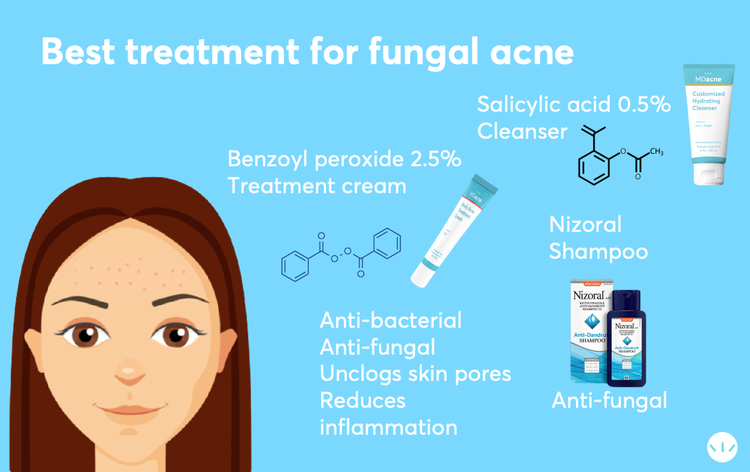
Over-the-Counter Fungal Acne Treatments
For many, **over-the-counter fungal acne treatments** can be effective. Look for creams containing active ingredients such as clotrimazole and ketoconazole, which have proven benefits in combating fungal infections. **Antifungal creams for acne** can decrease proliferation of yeast and aid in healing affected areas. Combine these topical routes with daily cleansing to ensure debris does not contribute to further flare-ups.
Professional Treatments for Fungal Acne
If over-the-counter options don’t yield results, you might consider professional treatments. Dermatologists can prescribe stronger **effective fungal acne medications** or recommend specific procedures involving light therapy, which can manage stubborn cases. Staying updated on alternative treatments can enhance your skincare relationships, helping tailor a routine that better suits individual skin needs.
Tips for Treating Fungal Acne at Home
Alongside external treatments, maintaining proper personal hygiene and skincare practices is paramount. Here are several **tips for treating fungal acne** at home:
– **Maintain cleanliness**: Regularly cleanse your skin with a gentle, antifungal body wash to minimize yeast buildup.
– **Use breathable fabrics**: Opt for loose-fitting clothing made from natural fibers to discourage yeast overgrowth.
– **Implement a nourishing routine**: Hydrate your skin well without using pore-clogging products. Seek **fungal acne safe ingredients** such as aloe vera and tea tree oil.
Fungal Acne Skincare Routine
Crafting the right **fungal acne skincare routine** can impact overall skin health. Following a consistent regimen tailored for fungal acne will help manage symptoms effectively. Start with a thorough facial cleanser to remove impurities.
Cleansing Routine for Fungal Acne
A diligent **cleansing routine for fungal acne** is essential. Use a sulfate-free cleanser designed for oily or combination skin to avoid irritation. Follow this with a mild exfoliant 1-2 times weekly to remove dead skin cells. Finish with a lightweight, **oil-free moisturizer** that won’t clog pores. Look into **best products for fungal acne** endorsed by dermatologists for optimal results.
Fungal Acne Diet Tips
Your diet can significantly affect fungal acne conditions. Some foods may promote yeast growth, while others can help curb it. Emphasize a diet rich in fresh vegetables, lean proteins, and whole grains, while minimizing sugar and refined carbohydrates. Examine **fungal acne and diet** connections by keeping a food journal to identify any triggers in your eating habits.
Everyday Habits to Prevent Fungal Acne
Preventing fungal acne involves small daily choices. Ensure proper sun protection to avoid skin damage that can promote yeast overgrowth. Adapt your exercise habits by showering immediately after physical activities to remove sweat that can breed yeast. These **everyday habits to prevent fungal acne** can create a significant impact over time.
Key Points for Effective Management
Managing fungal acne effectively requires a multifaceted approach, combining skincare routines, dietary considerations, and proper lifestyle changes. Follow trending fungal acne solutions that include consistent application of antifungal treatments in conjunction with personal habits aimed at balancing skin microbiome health. Tracking your **fungal acne recovery timeline** can keep you motivated on the path toward clear skin.
Fungal Acne and Lifestyle Changes
Several **lifestyle factors impacting fungal acne** include stress, climate, and daily routines. It’s vital to identify potential triggers in one’s life that exacerbate the condition. Staying hydrated, getting enough rest, and practicing stress-relief techniques are effective strategies for maintaining skin wellness in the face of fungal acne challenges.
Education and Community Support on Fungal Acne
Being educated about fungal acne and knowing you’re not alone can ease some emotional burdens. Engage with **fungal acne discussion forums** to share experiences and gain insights from others who have tackled similar issues. Learning from the experiences of many can provide support and new strategies for effective management.
Fungal Acne Care Guide Conclusion
Fungal acne can be managed with proper knowledge, lifestyle changes, and clinical assistance when necessary. Whether you struggle with **managing fungal acne** due to environmental factors or personal care choices, understanding and addressing the condition holistically can lead to positive improvements and renewed confidence.
FAQ
1. What are the best antifungal products for fungal acne treatment?
The best antifungal products for treating fungal acne include creams with ingredients such as ketoconazole and clotrimazole. These are effective in combating the yeast responsible for fungal acne. Additionally, some individuals find success with fungal acne-specific skincare lines that focus on **fungal acne safe ingredients**.
2. How can diet influence fungal acne?
Diet plays a crucial role in managing fungal acne. High sugar and refined carbohydrate intake can feed yeast overgrowth. Therefore, consuming a balanced diet of vegetables, proteins, and whole grains while avoiding high-sugar foods can help keep fungus levels in check.
3. How long does it typically take to treat fungal acne?
The timeline for **how long to treat fungal acne** can vary depending on the treatment methods used and the skin’s response. Generally, you can expect to see improvement within 4 to 6 weeks if the proper antifungal methods and skin care regimes are maintained consistently.
4. What signs should I look for to determine if my fungal acne is improving?
Signs of improvement in fungal acne can include reduced itchiness, fewer breakouts, and diminished redness and swelling. By keeping a **skin journal**, you can monitor changes over time, which is particularly beneficial during treatment.
5. Can stress exacerbate fungal acne?
Yes, stress is a known trigger that can worsen fungal acne by impacting the skin’s microbiome and functionality. Regular stress management practices can make a significant difference in reducing flare-ups of fungal acne.
6. Are professional treatments necessary for stubborn fungal acne?
While many cases of fungal acne can be managed with over-the-counter treatments, professional treatments may be necessary for stubborn cases. Dermatological advice can help in choosing the most effective **treatments for fungal acne**.
“`